The Therapeutic Role of Metatarsal Pads in Treating Foot Problems
The human foot is a remarkable structure, comprising 26 bones, 33 joints, and over 100 muscles, tendons, and ligaments working in concert to support body weight, absorb shock, and facilitate movement. Despite this sophisticated engineering, the foot remains vulnerable to numerous conditions that can compromise function and cause significant discomfort. Among the various conservative treatment options available, metatarsal pads have emerged as a simple yet effective intervention for addressing a range of foot pathologies. These unassuming devices, when properly applied, can provide substantial relief and functional improvement for patients suffering from forefoot pain and related conditions.
Metatarsal pads, also known as met pads, are small cushioning devices typically made from foam, gel, or felt materials. They are designed to be placed just proximal to the metatarsal heads—the rounded ends of the long bones in the forefoot that form the ball of the foot. Unlike metatarsal cushions, which pad the area directly beneath the metatarsal heads, metatarsal pads are positioned slightly behind these structures. This strategic placement serves a specific biomechanical purpose: to redistribute pressure away from painful areas, elevate and spread the metatarsal heads, and restore more natural foot mechanics during weight-bearing activities.
The primary mechanism by which metatarsal pads achieve therapeutic benefit involves pressure redistribution and mechanical realignment. During normal gait, the metatarsal heads bear significant forces during the push-off phase of walking. When certain conditions develop—such as metatarsalgia, Morton's neuroma, or fat pad atrophy—these forces can become concentrated in ways that produce pain and dysfunction. By placing a pad just behind the metatarsal heads, the device effectively creates a fulcrum that slightly elevates the metatarsals and encourages weight distribution across a broader surface area. This reduces peak pressures on any single point and can alleviate symptoms associated with overloading specific structures.
Metatarsalgia, a general term describing pain in the ball of the foot, represents one of the most common indications for metatarsal pad use. This condition can arise from various factors including high-impact activities, ill-fitting footwear, foot deformities, or excessive body weight. Patients typically report a sharp, aching, or burning sensation in the forefoot that worsens with standing or walking. Metatarsal pads address this condition by reducing concentrated pressure on inflamed or irritated tissues, allowing them to heal while the patient maintains normal activity levels. Clinical studies have demonstrated that proper use of metatarsal pads can significantly reduce pain scores and improve functional outcomes in metatarsalgia patients.
Morton's neuroma, a thickening of nerve tissue between the metatarsal heads—most commonly between the third and fourth toes—responds particularly well to metatarsal pad therapy. This condition produces symptoms including sharp shooting pain, burning sensations, numbness, or the feeling of standing on a pebble. The neuroma develops when nerves become compressed and irritated by the surrounding structures, particularly the transverse metatarsal ligament. Metatarsal pads work by spreading the metatarsal heads apart, reducing compression on the affected nerve. This mechanical decompression can provide immediate symptomatic relief and, in some cases, may prevent progression of the condition, potentially avoiding the need for corticosteroid injections or surgical intervention.
Fat pad atrophy, a condition particularly common in older adults, occurs when the protective cushioning under the metatarsal heads diminishes over time. This natural aging process leaves the metatarsal heads more vulnerable to impact forces during walking. Metatarsal pads compensate for this lost cushioning by providing external support and redistributing forces. For elderly patients who experience pain with each step due to inadequate natural padding, properly fitted metatarsal pads can dramatically improve mobility and quality of life.
Patients with claw toes, hammer toes, or bunions may also benefit from metatarsal pad therapy. These structural deformities often alter normal foot mechanics, leading to abnormal pressure distribution and secondary metatarsalgia. While metatarsal pads cannot correct the underlying deformity, they can mitigate painful symptoms by optimizing pressure distribution and may slow the progression of associated complications.
The effectiveness of metatarsal pad therapy depends critically on proper placement and sizing. Incorrectly positioned pads can exacerbate symptoms or create new problems. The pad should be located just proximal to the metatarsal heads, not directly beneath them. Finding the optimal position often requires trial and adjustment, as individual foot anatomy varies considerably. Podiatrists and physical therapists can provide guidance on proper placement techniques, and patients should be prepared to experiment with minor adjustments to achieve maximum benefit.
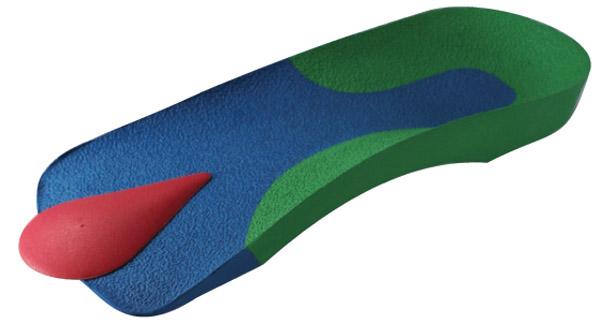
Metatarsal pads come in various forms, each with distinct advantages. Adhesive pads attach directly to the foot or the insole of shoes, maintaining consistent positioning. Non-adhesive pads incorporated into insoles or orthotics offer convenience and durability. The material choice—whether gel, foam, or felt—affects both comfort and durability. Softer materials may provide superior initial comfort but compress more quickly, while firmer materials offer longer-lasting support but may require an adaptation period.
Integration with appropriate footwear represents another crucial factor in successful treatment. Shoes with adequate depth in the toe box, good arch support, and rigid soles complement metatarsal pad therapy. Conversely, high heels, tight shoes, or footwear with insufficient cushioning can negate the benefits of even properly placed pads. Patients should be counseled about footwear choices as part of a comprehensive treatment approach.
While metatarsal pads offer significant benefits, they are rarely a standalone solution. Most effective treatment protocols incorporate multiple interventions including activity modification, stretching exercises, strengthening programs, anti-inflammatory measures, and appropriate footwear. Metatarsal pads work synergistically with these modalities to provide optimal outcomes.
Metatarsal pads represent a valuable conservative treatment option for various forefoot pathologies. Their relatively low cost, ease of use, and minimal risk profile make them an attractive first-line intervention for conditions including metatarsalgia, Morton's neuroma, and fat pad atrophy. When properly selected, positioned, and integrated into a comprehensive treatment plan, these simple devices can provide substantial pain relief and functional improvement, allowing patients to maintain active lifestyles while avoiding more invasive treatments.
Post Your Ad Here

Comments