Finding Relief: The Role of Insoles in Managing Hallux Rigidus
Hallux rigidus, a degenerative arthritic condition affecting the big toe joint, represents one of the most common sources of foot pain in adults. This progressive disorder causes stiffness, pain, and reduced mobility in the metatarsophalangeal joint—the critical hinge where the big toe meets the foot. For the millions of people living with this condition, every step can become a painful reminder of their limited mobility. While surgical intervention remains an option for severe cases, conservative management through specialized insoles has emerged as a cornerstone of non-invasive treatment, offering significant relief and functional improvement for many patients.
Understanding the biomechanics of hallux rigidus is essential to appreciating why insoles can be so effective. The big toe joint normally bends upward approximately 65 degrees during the walking cycle, a motion called dorsiflexion that is crucial for proper gait. When arthritis develops in this joint, the smooth cartilage deteriorates, bone spurs form, and the range of motion becomes severely restricted. This limitation forces compensatory movements throughout the foot and leg, often leading to additional problems in the ankles, knees, and even the lower back. The pain typically worsens with activities that require toe extension, such as walking uphill, running, or even wearing shoes with elevated heels.
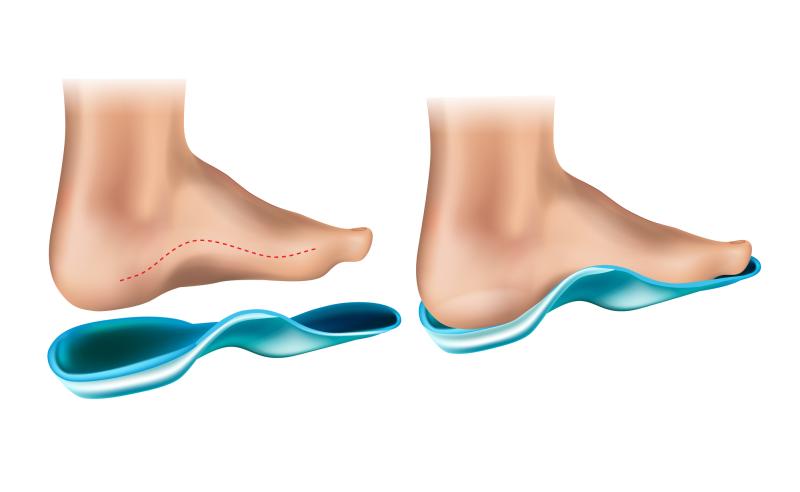
Therapeutic insoles designed for hallux rigidus work through several complementary mechanisms. The primary goal is to reduce the amount of bend required at the painful joint during walking. By incorporating a rigid extension under the big toe area—often called a Morton's extension or forefoot rocker—these insoles limit dorsiflexion while still allowing forward propulsion during gait. This modification fundamentally changes how forces are distributed across the foot, transferring pressure away from the arthritic joint and onto healthier areas that can better tolerate the load.
The construction of effective insoles for hallux rigidus typically involves multiple strategic elements. A firm shank or carbon fiber plate embedded in the forefoot region provides the structural rigidity necessary to prevent excessive toe bending. This stiffness must be carefully balanced—too rigid and the insole feels uncomfortable and unnatural; too flexible and it fails to provide adequate protection. Many advanced designs incorporate a rocker sole profile that curves the bottom of the insole, creating a rolling motion that helps propel the foot forward without requiring significant toe extension. This gentle rocking action mimics the natural gait cycle while minimizing stress on the compromised joint.
Cushioning represents another critical component of hallux rigidus insoles. Strategic padding beneath the ball of the foot helps absorb shock and reduce pressure on the metatarsal heads, which often bear excessive weight when normal toe function is impaired. Materials such as memory foam, gel, or specialized polymers conform to the foot's contours while providing resilient support. Some designs include a small relief area or cutout directly beneath the painful joint, further reducing direct pressure on the most tender spots.
Arch support also plays an important supporting role in these orthotic devices. Proper arch support helps maintain optimal foot alignment, preventing excessive pronation or supination that could place additional stress on the already compromised toe joint. By distributing forces more evenly across the entire foot, adequate arch support reduces the compensatory movements that often develop as patients unconsciously try to avoid painful toe motion.
The selection of appropriate insoles requires careful consideration of individual needs and disease severity. Over-the-counter options provide a cost-effective starting point for mild to moderate cases, with many manufacturers offering insoles specifically marketed for hallux rigidus or "turf toe." These prefabricated insoles come in various arch heights and rigidity levels, allowing some degree of customization. However, their one-size-fits-most approach may not adequately address complex foot structures or advanced disease stages.
Custom orthotic insoles, crafted by podiatrists or orthotists from precise molds or scans of the patient's feet, offer superior fit and targeted correction. These devices can be fine-tuned to address unique anatomical variations, accommodate other foot conditions, and provide graduated support that evolves as the condition progresses. While significantly more expensive than off-the-shelf alternatives, custom insoles often prove worthwhile for patients with moderate to severe symptoms or those who have found insufficient relief from commercial products.
Material selection significantly impacts both the performance and longevity of hallux rigidus insoles. Traditional materials like leather, cork, and rigid plastics have given way to advanced composites, carbon fiber, and medical-grade foams that offer superior durability and comfort. Some modern insoles incorporate multiple density layers, combining firm support where needed with softer cushioning in pressure-sensitive areas. Temperature-sensitive materials that mold to the foot's shape with body heat provide personalized comfort while maintaining necessary structural integrity.
The effectiveness of insoles depends heavily on proper footwear pairing. Shoes with adequate depth and width accommodate the added volume of orthotic insoles without creating pressure points. A stiff-soled shoe complements the insole's rigidity, further limiting toe joint motion. Conversely, flexible fashion shoes or minimalist footwear may undermine the insole's therapeutic benefits. Many podiatrists recommend shoes with rocker bottoms, which work synergistically with specialized insoles to create an optimal biomechanical environment for the compromised joint.
Clinical evidence supports the use of orthotic insoles as an effective conservative treatment for hallux rigidus. Studies have demonstrated significant improvements in pain levels, walking ability, and quality of life measures among patients using appropriate insoles. While these devices don't reverse the underlying arthritis, they can slow disease progression by reducing repetitive trauma to the joint. For many patients, proper insoles delay or even eliminate the need for surgical intervention, representing a valuable first-line treatment approach.
Specialized insoles represent a powerful tool in the management of hallux rigidus, offering meaningful relief through thoughtful biomechanical intervention. By limiting painful joint motion, redistributing pressure, and supporting proper foot alignment, these devices enable many patients to maintain active lifestyles despite their condition. Whether choosing over-the-counter or custom options, individuals with hallux rigidus should view insoles not as a simple comfort measure but as a therapeutic intervention worthy of careful selection and professional guidance.
Post Your Ad Here
Comments