Treatment of Haglund's Deformity
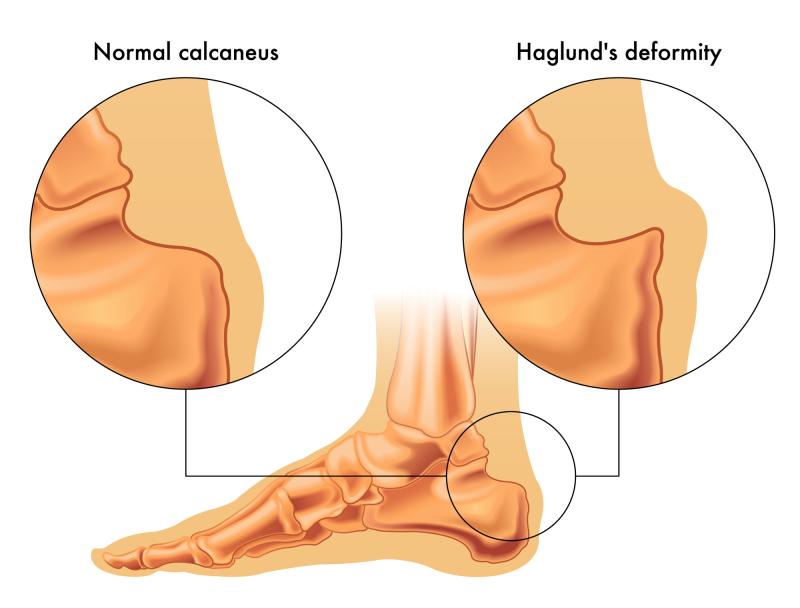
Haglund's deformity, commonly known as "pump bump," is a bony enlargement on the posterior aspect of the calcaneus where the Achilles tendon attaches to the heel bone. This condition causes significant discomfort and functional limitations for many individuals, particularly those who wear rigid-backed shoes. Understanding the various treatment approaches for this condition is essential for both patients and healthcare providers seeking to manage symptoms and restore normal foot function.
Understanding the Condition
Before exploring treatment options, it's important to understand what causes Haglund's deformity to develop. The condition involves a prominence of the posterosuperior calcaneal tuberosity, which creates friction between the heel bone, the Achilles tendon, and the overlying soft tissues. This friction leads to inflammation of the retrocalcaneal bursa (retrocalcaneal bursitis) and the superficial bursa between the skin and the Achilles tendon. The combination of bony prominence and soft tissue inflammation creates the characteristic pain and swelling associated with this deformity.
Several factors contribute to the development of Haglund's deformity, including inherited foot structure, high arches, tight Achilles tendons, and a tendency to walk on the outside of the heel. However, the condition is often exacerbated by footwear choices, particularly shoes with rigid heel counters that press against the bony prominence.
Conservative Treatment Approaches
The vast majority of patients with Haglund's deformity can be managed successfully with conservative, non-surgical treatments. These approaches focus on reducing inflammation, minimizing friction, and addressing biomechanical factors that contribute to symptoms.
Modification of footwear represents the first line of treatment. Patients are advised to avoid shoes with rigid heel counters and instead choose footwear with soft, flexible backs or open-heeled shoes such as clogs or sandals. Some individuals find relief by using heel lifts or pads that elevate the heel slightly, changing the angle at which the Achilles tendon pulls on the calcaneus and reducing pressure on the prominent area. Custom orthotic devices may also be prescribed to control abnormal foot mechanics and reduce stress on the heel.
Physical therapy plays a crucial role in conservative management. Stretching exercises targeting the Achilles tendon and calf muscles can reduce tension on the heel attachment point. A tight Achilles tendon increases the pressure and friction at the insertion site, so improving flexibility can provide significant relief. Physical therapists may also employ ultrasound therapy, iontophoresis, or other modalities to reduce inflammation in the affected tissues.
Ice therapy is a simple yet effective method for managing acute flare-ups of pain and swelling. Applying ice to the affected area for 15 to 20 minutes several times daily can help reduce inflammation and provide symptomatic relief. Anti-inflammatory medications, both oral and topical, are commonly used to manage pain and reduce swelling in the bursal tissues and surrounding soft tissues.
Immobilization may be necessary in more severe cases. A walking boot or cast can be used temporarily to completely rest the affected area and allow inflammation to subside. While this approach is more restrictive, it can be highly effective for patients who have not responded to other conservative measures.
Corticosteroid injections are sometimes considered for patients with persistent bursitis, though they must be administered with caution. Injections are typically directed into the retrocalcaneal bursa rather than near the Achilles tendon itself, as steroid exposure can weaken tendon tissue and increase the risk of rupture. This treatment option is generally reserved for cases where other conservative measures have failed and is used judiciously.
Surgical Treatment Options
When conservative treatments fail to provide adequate relief after several months, surgical intervention may be considered. Surgery for Haglund's deformity aims to remove the bony prominence, reduce pressure on the surrounding soft tissues, and alleviate chronic inflammation.
The most common surgical procedure is an osteotomy, which involves reshaping the posterior calcaneus by removing the prominent portion of bone. This procedure, often called a calcaneal exostectomy, reduces the mechanical irritation that causes bursal inflammation. Surgeons may perform this procedure using traditional open techniques or, in some cases, minimally invasive approaches.
During surgery, the inflamed retrocalcaneal bursa is typically removed (bursectomy) along with any inflamed tissue surrounding the Achilles tendon. In some cases, if the Achilles tendon has sustained damage from chronic inflammation, the surgeon may need to debride or repair the tendon. Severe cases may require detachment and reattachment of the Achilles tendon to allow adequate access to the bony prominence, though this is less common with modern surgical techniques.
Recovery from surgery typically involves a period of immobilization in a cast or boot, followed by gradual rehabilitation. Patients can usually bear weight on the affected foot within a few weeks, though return to normal activities may take several months. Physical therapy is essential during the recovery period to restore strength, flexibility, and normal gait patterns.
Surgical outcomes are generally favorable, with most patients experiencing significant pain relief and improved function. However, as with any surgical procedure, there are risks including infection, nerve damage, wound healing complications, and in rare cases, Achilles tendon rupture. Additionally, some patients may experience recurrence of the prominence, though this is uncommon with proper surgical technique.
Haglund's deformity is a challenging condition that can significantly impact quality of life, but effective treatment options exist for most patients. The conservative approach, emphasizing footwear modification, physical therapy, and anti-inflammatory measures, successfully manages symptoms in the majority of cases. For those who do not respond to conservative care, surgical intervention offers excellent outcomes with relatively low complication rates. The key to successful treatment lies in early recognition of the condition, appropriate initial management, and patient education about factors that contribute to symptoms. With proper care, most individuals with Haglund's deformity can achieve lasting relief and return to their normal activities without significant limitations.
Post Your Ad Here

Comments