Why UK care homes struggle to meet needs of dementia residents
Care
homes in the UK are struggling to provide satisfactory care to residents living
with advanced dementia, new research has revealed.
Dementia
Awareness Week plans to raise understanding of the frequently heartbreaking
process of attempting to get NHS financing
Faced
with limited spending plans, the Gateway care home in Bradford, England thought
of a strange answer for getting residents all over the place — a mock
eight-seater train carriage takes them on a simulated adventure that happens on
two video screens a few times each day.
"Trains
experience everybody's memory" says, Chris White. "Many numbers of
our residents can't get out or it's costly, so we figured out of another method
for giving people opportunities.
Mr
White’s approach underscores the trouble care homes face supporting the rising number of residents with dementia and other acute conditions.
In
spite of the fact that the government encourages the older to stay in their
very own homes, this implies care homes are progressively receiving patients
just once they have chronic or end-of-life conditions that require all the more
nursing.
The
Alzheimer's Society says 70 percent of UK care home residents have dementia or
serious memory issues, adding to money-related pressures.
The report found that low staff confidence and insufficient training have left care
homes staff unable to perceive and react to the complex needs of residents with
advanced dementia, similarly, NHS administrations, for example, hospitals do.
"The
research has featured that care home staff might not have the right skills to
perceive when somebody with dementia is in the later phases of the condition or
at the end-of-their life.
The UK cost
of dementia is accepted to rise significantly
Not all homes can charge more, either from residents
or state authorities. This leaves many struggling or cutting exercises that
assist fight with offing mental decline.
In excess of 400 care home, operators have collapsed
since 2010, as per Care England, leaving a total today of around 5,000 over The UK.
There is set to be a shortfall of 30,000 care home
spots for people with dementia by 2021, as indicated by the Alzheimer's
Society.
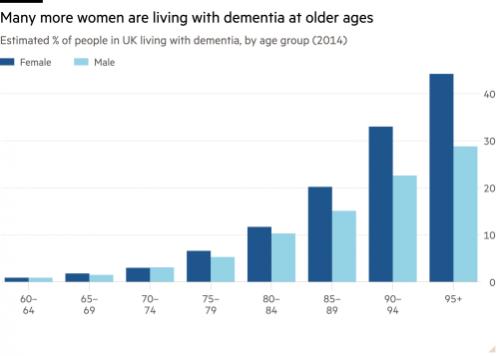
A lot more
women are living with dementia at older ages
Moreover, the Care Quality Commission found that the fifth of homes in England neglected to fulfill even the least guidelines a year
ago.
Robert Kilgour, the owner of Renaissance Care, has
seen an expansion in levels of dependency.
"Residents with dementia are similarly prone to
be up in the center of the night as during the day, so you need more staff with
more experience with all hours," he says.
But finding workers — which accounts for two-thirds of
costs-is a perennial issue in the industry depending on low pay and zero-hours
contracts.
Cuts in nurse training spending plans, increasingly
restrictive immigration strategies and increases to the lowest pay permitted by the law have heaped on extra pressure.
Alzheimer's is a terminal condition but it doesn't get
the extra NHS funding got by patients with illnesses, for example, cancer —
despite the fact that the expenses of a care home spot for people with dementia
will, in general, be £200 to £300 per week higher than for those without.
"The policies are short-terms as they mean more
people are forced into the hospital, which is the more costly choice," she
adds.
Care homes cope with the additional expenses by
energizing to 40 percent higher charges to self-funders, which subsidizes
state-funded residents. This, in any case, puts a horrendous burden on numerous
families that struggle to pay for care.
In spite of the money related pressures, numerous
homes stay profitable, with an immense hole between those that depend on
lucrative private-payers and those that rely upon local authority expenses.
The finances of these offshore-owned companies are
obscure but HC-One has paid out at any rate of £48.5m in profits in the
previous two years in spite of arguing for all the more funding from the
government.
A few owners and the unreasonably high-interest rates
charged on loans by certain financiers are totally wrong for what ought to
always be public and not a business administration."
"There is, by and large, poor knowledge of how
best to manage common symptoms in people with advanced dementia. There are
different reasons behind this breakdown in care but the discoveries suggest
that an increasingly integrated, multidisciplinary approach that improves the
communication between all the care suppliers involved would achieve
improvement. Be that as it may, the funding and assets should be accessible and
for this, there should be more recognition and commitment from policymakers."
The report revealed boundaries to demonstrating
high-quality care, this included: separation from the more extensive wellbeing
and social care framework and an absence of access to specialist help, for
example, end-of-life care administrations.
Figures from Alzheimer's Society demonstrate that 80
percent of UK care home residents have dementia or another type of
psychological disability, while most of the people with dementia in the UK will
pass on while living in a care facility.
People living with advanced dementia could turn out to
be doubly incontinent, unable to communicate their needs and have different
co-morbidities, for example, diabetes and hypertension. Just as being at
expanded risk of hospitalization after chest, urinary tract infections and
experience visit pain, anxiety, and swallowing issues.
Care home
revolution
"We
urgently need a care home revolution to change the nature of the care and
support gave. The workforce ought to be well-trained and put resources into, on
a standard with the NHS, and not a poor relation." The study uncovered
that numerous respondents accept that the UK Government system, increasing
governance of care processes constrained funding and the business-focused
nature of care homes, all take away from the nature of care being given to
residents propelled dementia. While wellbeing and social care commissioners
stay concentrated on issues identifying with the beginning periods of dementia.
We
need better communication and relationships between care experts and benefits,
and improved preparing with the goal that cares home staff can tell when
somebody is in the later phases of the condition or moving the end of their
life."
So,
Downsvale Nursing Home center
doesn't fail for giving treatment for elderly people who suffer from dementia
and Alzheimer's. Nursing home in
Guildford works to improve the quality of life of people affected by
dementia and has an office in Surrey,
Dorking, UK.
It
is a Specialist Nursing and Dementia care and community for the elderly in
Dorking, Surrey.
You
will find peace of mind knowing that your loved one is receiving the best
possible nursing care in a loving and understanding place. With delightful views to the Box Hill AONB,
Downsvale is the perfect place for people with Nursing and Dementia needs to
experience the best possible life!
The home provides a specially designed environment to suit people with Nursing and
Dementia needs. For example, we provide specialist nursing equipment such as
nursing beds, pressure care mattresses, etc., to support our resident’s nursing
needs.
You
are most welcome to pop in and take a look around. If you have any questions or
would like to arrange an appointment with the Home Manager for a confidential
chat about your requirements please call us on 01306772220 | 01306887652 OR Visit: https://www.downsvale.co.uk/
Post Your Ad Here
Comments