Medical Billing Processes - Why Secure FTP Services Are Required For the Medical Billing Process
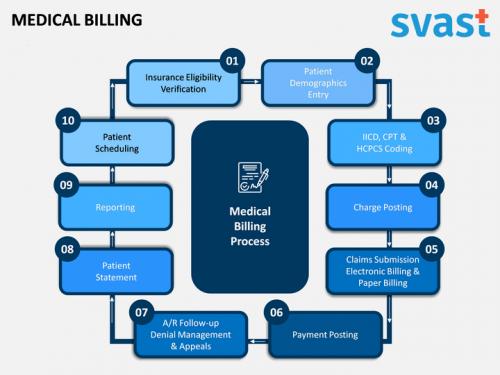
Medical
billing is an administrative payment procedure within the U.S.
health care system. The process entails a health care provider submitting,
within a certain time frame, claims for services rendered to medical insurance
companies so that they can pay for these services; including tests, treatments,
and diagnostics performed by medical professionals. When a claim is received
from a doctor or hospital within this administrative process, it is referred to
as an "insured claim." From there, an invoice is sent to the
insurance carrier or organization that provided the service. This invoice
contains information regarding the amount of service billed, what was done, who
paid what, the date on which the bill was generated, etc.
In the end,
an account is created. This account is used by the medical billing and coding
organization to keep track of all of these individual claims and payments.
Medical billers and coders then enter the data within their systems, and assign
a percentage to each claim. From this percentage, a payment is generated for
the service rendered. As the health insurance company receives the payment,
they then retain the right to verify that the amount of coverage was correctly
stated, or if errors occurred and need to be corrected.
Medical
billing and coding organizations are also responsible for sending
patient visits to doctors and hospitals. At this point, the relationship
between the patient and the health care provider becomes defined. Medical
billing and coding organizations also prepare pre-authorization forms for
individuals to sign if they require extended health care. As an organization,
the primary function of the medical biller is to ensure all of the necessary
procedures are completed to the patients' satisfaction. Therefore, it is
important that the medical bills remain organized. A well-organized medical
coder and biller will ensure that each patient visit is processed correctly to
prevent any issues later on.
Medical
billing and coding organizations must maintain patient records at all times, or
the practice could be held accountable for any errors that arise. If the healthcare
provider is not connected to the healthcare system at all times, it is
essential that they hire an independent third party company that can meet the
needs of this unique healthcare industry. Outsourcing medical billers and
coders is one of the most important business decisions that any healthcare
facility can make.
One of the
most common tasks that these companies perform is medical records management.
Medical billing and coding require that they maintain accurate information
about patient records. This means that they must be able to organize records
from different sources, such as insurance, government, private insurance,
private health agencies and the International Classification of Diseases and
Health Problems (ICD and HCV) into a standard database. The accuracy of this
database is necessary in order for the health care professional to process and
receive appropriate payment for the services rendered.
A secure ftp
software is required in order to complete this medical billing process. Most
practices are aware of the benefits of outsourcing this function to a third
party company. There are some advantages to doing so, such as the ability to
save money on having to maintain the company's own infrastructure and the
ability to increase profits because the business will pay a lower monthly fee
for storing and processing patient data. However, there are many disadvantages
to outsourcing the medical billing process, including the risk of errors caused
by human error. Many professionals in the healthcare industry underestimate the
importance of maintaining the accuracy of their data, because it is considered
a minor detail when compared to implementing effective systems for billing and
coding.
Post Your Ad Here

Comments