Arthritis: Causes, Symptoms & Treatment
by James Denlinger Digital Marketing StrategistArthritis is a general term for a variety of disorders that cause swelling, stiffness, joint pain and restricted motion. About 50 million adults have arthritis, making it the second leading cause of disability in the United States. There are over 100 types of arthritis, ranging from symptoms that are only mildly painful to completely incapacitating. Osteoarthritis (OA), rheumatoid arthritis (RA) and psoriatic arthritis (PA) are the most common forms of adult arthritis. At the onset, arthritis pain may be limited to a single joint, but over time it can spread to other areas. It may also impact the lungs, kidneys and skin.
Arthritis can develop as a result of many different conditions — from disease processes, to injuries, to aging. Rheumatoid and psoriatic arthritis are both caused by an immune system response, whereas osteoarthritis results from wear-and-tear of joints. Any condition that puts excessive stress on joints can result in arthritis. Even healthy exercise like walking and running can place too much stress on joints.
Types of Arthritis
Knowing the hallmarks of each type of arthritis can help identify the condition. But visiting a physician is the best way to identify arthritis. The most common forms in adults are osteoarthritis, rheumatoid arthritis and psoriatic arthritis.
Osteoarthritis (OA)
Osteoarthritis occurs frequently and it’s the single most common joint disorder. Primary OA is caused by accumulated damage to joint cartilage. Cartilage is the hard flexible coating that caps the ends of bones and allows the joints to move. It wears down over time and with damage, leading to painful and restrictive bone-to-bone contact. It can also derive from bone microfractures caused by bone-to-bone impacts.
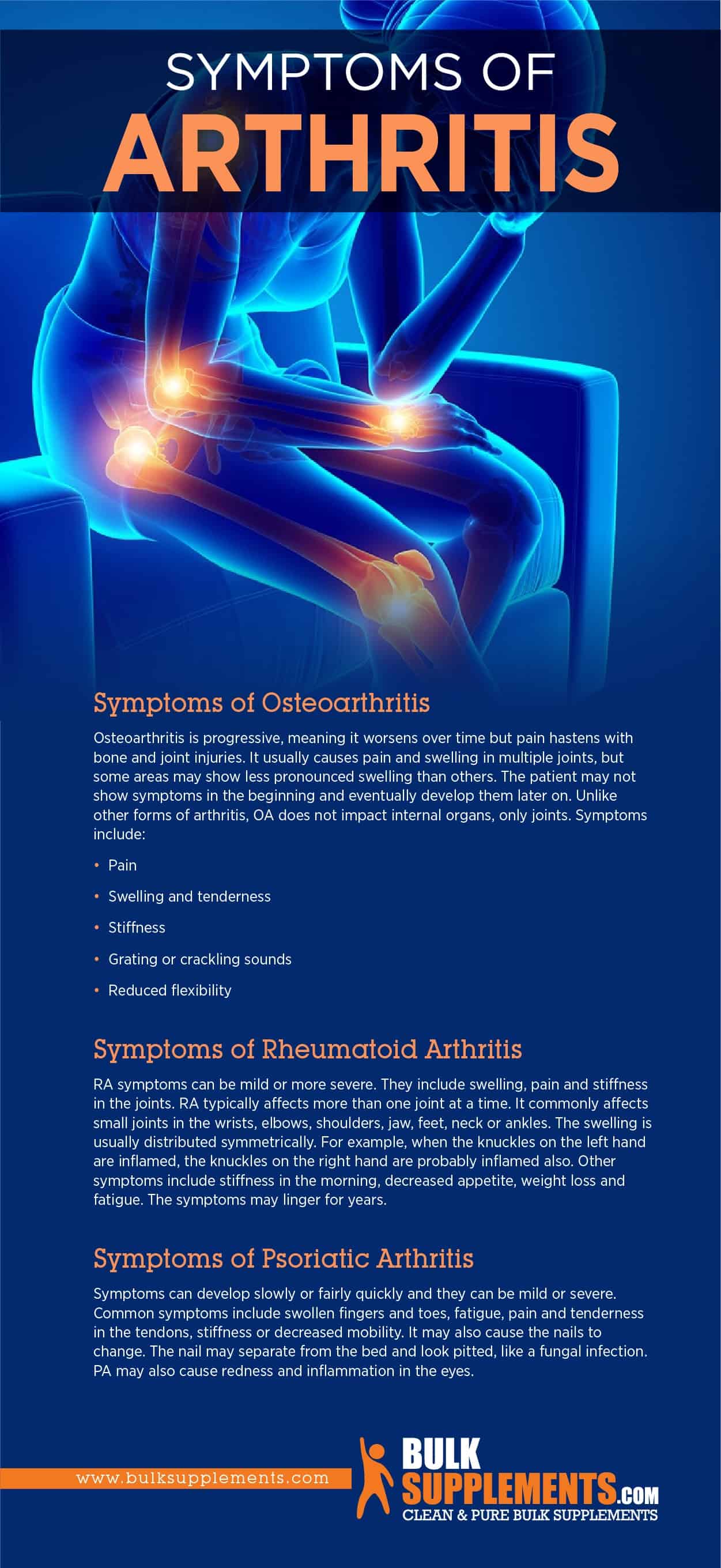
Symptoms of Osteoarthritis
Osteoarthritis is progressive, meaning it worsens over time but pain hastens with bone and joint injuries. It usually causes pain and swelling in multiple joints, but some areas may show less pronounced swelling than others. The patient may not show symptoms in the beginning and eventually develop them later on. Unlike other forms of arthritis, OA does not impact internal organs, only joints. Symptoms include:
- Pain
- Swelling and tenderness
- Stiffness
- Grating or crackling sounds
- Reduced flexibility
Causes of Osteoarthritis
OA is most common in the elderly, specifically primary OA. Over time, joint cartilage degenerates because it cannot repair itself as effectively. There is no specific cause for primary osteoarthritis, but it is mostly related to age.
Secondary arthritis, on the other hand, has a cause other than just wear and tear. It can result from trauma, injury, surgery, obesity or genetics. Gout and diabetes are also common causes of secondary OA.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune disorder, in which the immune system attacks the synovial membrane that surrounds the joints, causing irritation and inflammation. Pain is often severe. Eventually, rheumatoid arthritis attacks both bone and cartilage. Rheumatoid arthritis causes swollen and inflamed joints. Nodules will typically form on the knuckles, heels or elbows. Rheumatoid arthritis flare-ups tend to be more severe than OA and can lead to disability.
Symptoms of Rheumatoid Arthritis
RA symptoms can be mild or more severe. They include swelling, pain and stiffness in the joints. RA typically affects more than one joint at a time. It commonly affects small joints in the wrists, elbows, shoulders, jaw, feet, neck or ankles. The swelling is usually distributed symmetrically. For example, when the knuckles on the left hand are inflamed, the knuckles on the right hand are probably inflamed also. Other symptoms include stiffness in the morning, decreased appetite, weight loss and fatigue. The symptoms may linger for years.
Stages of Rheumatoid Arthritis
RA progresses in four stages, each with different courses for treatment.
- 1st Stage: Joint and synovial tissue first begins to swell and patient starts to feel pain and stiffness.
- 2nd Stage: Synovial inflammation worsens and damages cartilage and the patient begins to lose mobility.
- 3rd Stage: This is severe RA. Inflammation beings to destroy bones along with cartilage. Pain and swelling increase and the patient loses more mobility. It may also cause deformities in the joints.
- 4th Stage: At this stage, the patient still feels pain, swelling and stiffness. But the joints stop functioning completely.
Causes of Rheumatoid Arthritis
The exact causes of RA remain unknown. But there are several factors that may play a role. Genetics may contribute, as well as gender and age. It is more common in women and in individuals between the ages of 40 and 60. Scientists think that there may be environmental factors as well. For example, bacterial or viral infections may cause the immune system to mistakenly identify joint tissue as an invading pathogen that it must destroy. Exposure to certain chemicals, air pollutants and second-hand smoke may also increase the risk.
Rheumatoid arthritis is also associated with celiac disease, an autoimmune disorder aggravated by gluten. Research identifies increased autoimmune diseases in celiac patients.
Psoriatic Arthritis (PA)
Psoriatic arthritis is common in patients with psoriasis, which is an autoimmune disease, in which the immune system attacks healthy skin cells and causes them to grow abnormally fast. Some psoriasis patients develop PA, but not all of them. Some people develop psoriatic arthritis if they do not even have psoriasis.
Causes of Psoriatic Arthritis
Like rheumatoid arthritis and the skin disorder psoriasis, psoriatic arthritis is an auto-immune disorder that develops when the immune system misidentifies proteins in the synovial membrane and mistakes them for pathogens.
Scientists do not know exactly what causes the identification error, but they have identified several risk factors (x). It is most common in people with psoriasis or those with a family history of it. People between 30 and 50 are more likely to develop PA. The symptoms worsen when the patient is exposed to specific triggers, such as infections, skin wounds, stress and certain medications.
Symptoms of Psoriatic Arthritis
Symptoms can develop slowly or fairly quickly and they can be mild or severe. Common symptoms include swollen fingers and toes, fatigue, pain and tenderness in the tendons, stiffness or decreased mobility. It may also cause the nails to change. The nail may separate from the bed and look pitted, like a fungal infection. PA may also cause redness and inflammation in the eyes.
 PIN IT
PIN ITComplications of Arthritis
Arthritis is most dangerous when it is left untreated. Untreated cases can cause damage to other parts of the body, not just the joints. Complications can include:
- Decreased movement, loss of function and disability
- Osteoporosis
- Joint destruction and deformity
- Kidney problems
- Heart disease
- Joint destruction and deformity
- Anemia
- Depression
- Cognitive dysfunction
- Spinal cord progression
Preventing Arthritis
There is no definite way to prevent arthritis, but it is possible to reduce the risks. Lifestyle choices can be a proactive way to minimize joint damage. First, maintaining a healthy weight can reduce the risk of osteoarthritis. Being overweight puts more pressure and stress on the joints and excess fat destroys joints and cartilage faster. Smoking tobacco is also a risk factor for rheumatoid arthritis, so avoiding cigarettes can reduce the risk. Rheumatoid arthritis is an autoimmune disorder and research states that smoking causes oxidative stress in the body, which impacts the immune system.
Treating Arthritis
One way to treat arthritis is with medication to help alleviate pain and inflammation in an arthritic flare-up.
Analgesics
Analgesics reduce pain. Acetaminophen and opioid-class narcotics are examples of analgesic drugs. Opioids require a prescription, but acetaminophen is available over the counter.
Nonsteroidal Anti-Inflammatory Drugs (NSAID)
NSAIDs reduce inflammation, pain and stiffness for arthritis and other similar disorders, such as tendinitis and bursitis. They come in several over-the-counter varieties, including naproxen sodium and ibuprofen.
Corticosteroids
These are effective anti inflammatory drugs, chemically similar to cortisol, which is a natural anti inflammatory in the body. They are also immunosuppressive and treat rheumatoid arthritis, osteoarthritis, lupus, asthma and allergies.
Disease-Modifying Antirheumatic Drugs (DMARD)
These drugs restrict the immune system and block inflammation to preserve the joints. However, they will not ease arthritic pain.
Surgical Procedures
Patients may also undergo surgery if the condition becomes debilitating. Common surgeries include arthroscopy, joint resurfacing and osteotomy. Arthroscopy uses a small camera to fix tears in the joint tissue, joint resurfacing replaces the joint and osteotomy removes or adds bone to a damaged joint.
Supplements for Bone & Joint Health
Supplements can act as natural remedies or treatment options for arthritis symptoms. They can help support bone and joint health and reduce inflammation, but supplements should not replace traditional treatment options. Consult a physician before implementing supplements into your diet and follow all of the physician’s instructions.
Boswellia
Known as Indian frankincense, boswellia reduces inflammation in osteoarthritis and rheumatoid arthritis. As a dietary supplement, take 450 mg once or twice daily, unless a physician orders otherwise.
Methylsulfonylmethane (MSM)
MSM is a powerful anti-inflammatory and it assists antioxidants and antibodies in the immune system. As a dietary supplement, take 1,000 to 1,300 mg four times a day, or as directed by a physician.
Hyaluronic Acid Powder
Occurring naturally in the body, hyaluronic acid helps keep aging cartilage hydrated and lubricated and supports the joints from extra pressure. It can help treat osteoporosis. Take 100 mg servings twice a day.
Bamboo Extract Powder
Bamboo extract may boost collagen production and bone growth. Collagen is a vital necessity for the health of the synovial membranes around the joints. As a dietary supplement, take up to 600 mg daily with water.
D-Glucosamine Sulfate Potassium Powder
Derived from shellfish, D-glucosamine supports bone and joint health. It may reduce pain and slow joint cartilage erosion. As a dietary supplement, take 1,000 mg up to three times a day, unless a physician recommends otherwise. Pregnant or nursing women should consult a doctor before supplementing.
Calcium Citrate Powder
Because calcium is one of the most common nutrients in the human body, it’s extremely important to maintain calcium levels. Calcium citrate may promote bone health and help the immune system function regularly. Take 2,380 mg once or twice a day with meals or following a physician’s instructions.
Calcium Gluconate Powder
Calcium gluconate is a readily and easily absorbable form of calcium, vital for bone health and immune system function. As a dietary supplement, take 5,600mg once or twice daily, preferably with meals.
Calcium Ascorbate
Calcium ascorbate is a buffered form of vitamin C combined with calcium. Vitamin C helps with collagen production, which provides muscle flexibility and keeps bone and cartilage healthy. As a dietary supplement, take 300 mg to 1,000 mg up to three times every day, or as directed by a physician.
Potassium Chloride Crystallized Powder
People with rheumatoid arthritis tend to be deficient in potassium chloride because of the medications they take to treat the condition. Reducing sodium chloride intake and substituting potassium chloride may help stabilize potassium levels. It can be an efficient salt substitute, but consult with a physician before using potassium chloride for arthritis. The recommended dosage is 135 mg a day with food and water.
The Bottom Line
Arthritis is a painful disorder that causes inflammation, swelling and pain in the joints. The most common forms are osteoarthritis, rheumatoid arthritis and psoriatic arthritis. Rheumatoid and psoriatic arthritis are both autoimmune disorders, while osteoarthritis is typically caused by age-related wear and tear.
Symptoms can be mild or severe and potentially debilitating. Treatment includes pain medication or surgery for severe cases. There is no definite way to prevent arthritis, but lifestyle choices can make a big difference to reduce the risk. Supplements can also help to promote strong joints and bones in conjunction with medical treatment.
Sponsor Ads
Created on Mar 16th 2020 22:13. Viewed 392 times.