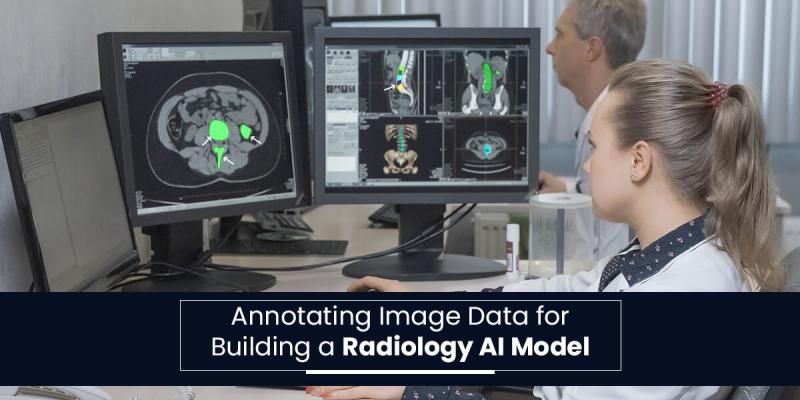
Annotating Image Data for Building a Radiology AI Model
In 2025, medical imaging is evolving beyond traditional X-rays and MRIs. The global medical imaging market is set for steady growth, with overall imaging volume projected to rise at a CAGR of 4.95% from 2025 to 2030. The burden of chronic disease and an aging population has led to an increase in the use of diagnostic imaging across care settings, supported by technological advances and greater access in emerging markets. Within this trend, advanced modalities such as CT and PET are expected to experience significant growth over the next decade, driven by their crucial role in early detection, treatment planning, and monitoring complex conditions, as well as speed, quality, and patient comfort improvements.
With the accelerating demand for image annotation, technology is advancing how images are analyzed. However, any AI model is only as good as the data on which it is trained. This marks the need for high-quality imaging data across modalities in radiology. For example, labeling organs, tumors, or fractures helps train AI systems effectively. Precise annotation ensures the AI learns correct patterns and minimizes diagnostic errors.
Radiology AI can minimize errors, enhance decision-making, and unlock new possibilities for understanding the human body and redefining patient care by leveraging robust data across modalities.
Here is a deep dive into the top types of medical data used for creating robust radiology AI models. Let’s explore:-
X-Rays
X-rays are the most widely used medical imaging technique worldwide. It is effective for initial screening and also serves as the basis for diagnostic imaging in hospitals, clinics, and resource-limited settings. Their standardized imaging protocols make them crucial foundations for developing and training radiology AI models.
Common Applications
Fracture detection – identifying subtle or complex bone injuries.
Lung diseases – spotting pneumonia, tuberculosis (TB), etc.
Oncology – detecting lung nodules that could indicate early-stage cancer.
Dental imaging – analyzing tooth alignment, cavities, or jaw abnormalities.
Bounding boxes or segmentation masks are often applied to fractures, nodules, and other major findings to train models in accurate detection.
Computed Tomography (CT) Scans
CT scans offer detailed cross-sectional and 3D visualization of the body. It provides more information than standard X-rays. These are vital for evaluating internal organs, blood vessels, organs, bones, and soft tissues, making them indispensable in oncology and surgical planning. CT stands as an essential modality for training AI systems to detect complex conditions, due to its ability to capture fine anatomical and pathological details.
Common Applications
Tumor detection and segmentation – identifying and measuring lung, liver, and brain cancers.
Stroke analysis – detecting ischemic and hemorrhagic strokes rapidly for time-critical interventions.
Trauma assessment – spotting fractures, internal bleeding, and organ injuries in emergency cases.
Lung disease evaluation – classifying nodules and interstitial lung disease from chest CT scans.
Segmenting organs, lesions, and tumors allows AI to learn precise anatomy and pathology patterns.
Magnetic Resonance Imaging (MRI)
MRI provides high-resolution, radiation-free imaging, making it ideal for visualizing soft tissues such as the brain, spinal cord, muscles, ligaments, and internal organs. Unlike X-rays or CT scans, MRI offers superior contrast between soft tissue types, critical for detecting subtle abnormalities, monitoring disease progression, and guiding surgical planning. Its versatility and safety make MRI a foundation in clinical diagnostics and AI research.
Common Applications
Neurological disorders – identifying lesions related to multiple sclerosis, Alzheimer’s disease, and stroke.
Brain tumors – automated segmentation, detection, and volumetric analysis for treatment planning.
Spinal cord and musculoskeletal injuries – evaluating disc herniation, ligament tears, and joint abnormalities.
Functional and quantitative imaging – analyzing perfusion, diffusion, and functional MRI data for advanced diagnostics.
Lesions and soft-tissue structures are labeled to train segmentation and classification algorithms.
Ultrasound
Ultrasound imaging technique uses sound waves instead of ionizing radiation, making it ideal for frequent and real-time monitoring. Its portability allows use at the bedside or in remote settings, which is especially useful in emergency care and resource-limited environments. Ultrasound is widely used in obstetrics and gynecology for monitoring pregnancy and in cardiology for assessing heart structure and function. It also works in emergency medicine for the rapid diagnosis of trauma and internal bleeding.
Common Applications
Fetal anomaly detection – Identifying structural abnormalities during prenatal scans.
Echocardiography – Measuring heart function, chamber sizes, and detecting cardiac diseases.
Liver and kidney scans – Detecting fibrosis, lesions, tumors, and other organ abnormalities.
Automated image acquisition – Guiding probe placement and optimizing scan angles for consistent quality.
Real-time decision support – Providing instant interpretation to assist clinicians in emergency or resource-limited settings.
Workflow efficiency – Reducing reporting time by auto-generating measurements and annotations.
Organ boundaries, fetal structures, and cardiac chambers are labeled to train real-time diagnostic models.
Mammography
Mammography is a diagnostic imaging technique used for the early detection of breast cancer. It is critical in reducing mortality by identifying suspicious changes in breast tissue, like calcifications or tumors, at an early and more treatable stage. Its use in routine screening programs worldwide has made it one of the most essential tools in women’s healthcare.
Common Applications
Tumor detection – Identifying suspicious masses that may indicate the presence of breast cancer.
Mass classification – Distinguishing between benign and malignant lesions to reduce unnecessary biopsies.
Microcalcification detection – Spotting tiny calcium deposits that can be an early sign of cancer.
Workflow support – Assisting radiologists with triaging cases, reducing false positives/negatives, and speeding up reporting.
Precise marking of tumors, calcifications, and suspicious regions improves detection and triaging models.
PET
Positron Emission Tomography (PET) is a powerful imaging modality. It provides functional and metabolic information alongside detailed anatomical context. It allows clinicians to visualize the structure of tissues and organs and also to assess their biological activity. PET scans are widely used in oncology for detecting tumors, monitoring treatment response, and staging cancer, as well as in neurology and cardiology for evaluating brain disorders and heart function.
Common Applications
Cancer staging and response monitoring – Accurately identifying tumor spread and assessing therapy effectiveness.
Alzheimer’s disease detection – Analyzing brain metabolism patterns for early diagnosis of neurodegenerative disorders.
Cardiology – Evaluating myocardial perfusion and viability to guide treatment planning.
Image Reconstruction and Noise Reduction – Enhancing Image Clarity with Lower Radiation Doses.
Radiomics and prognosis prediction – Extracting advanced imaging features to support personalized treatment decisions.
Metabolic regions of interest are marked to train models in detecting functional changes and disease progression.
Future Trends in Radiology
Radiology is divided into two main areas: diagnostic radiology and interventional radiology.
Diagnostic Radiology
Radiology needs to remain multi-directional, like the rest of medicine, as it works with contemporary scientific and technological advances. In the near future, this will evolve into the expanded use of hybrid imaging technologies, including PET/CT, as well as the integration of ultrasound into various procedures, such as robot-assisted interventions. Medical Image annotation will become predictive and highly personalized, a shift that is already underway.
The use of genetic biomarkers has already transformed treatment approaches for specific diseases, such as cystic fibrosis. In the coming decade and beyond, annotating images is likely to undergo rapid evolution as our understanding of metabolic processes continues to deepen. This knowledge will drive the development of novel tracers that can specifically identify these processes, boosting both the acquisition and application of clinical information.
These tracers will be developed not only for PET/CT but also for emerging MR/PET technology, which amalgamates the advantages of new tracers with the extensive capabilities of MR imaging sequences and MR spectroscopy. By integrating molecular imaging with genetic markers, radiology promises to provide even more robust tools for personalized medicine.
Interventional Radiology
Currently, interventional radiology is undergoing a state of transition. It utilizes accessible imaging modalities and combines them for better accuracy. Interventional radiology utilizes these techniques in conjunction with various treatment innovations, including radiofrequency, heat, and laser ablation devices. The improvement of catheters will transform body and neurointerventional radiology from a support-based service for improving vascular anomalies to a vital therapeutic tool in body and cerebral oncology. It enables precise interventions with the support of specialized medical expertise. The integration of genetic markers in radiology will further expand the role of image-guided procedures.
Conclusion
Data and personalized care drive the future of radiology. High-quality imaging across diverse modalities, combined with precise annotation, is crucial for training reliable AI systems to detect subtle abnormalities, minimize diagnostic errors, and inform clinical decision-making. Specialized annotation services ensure quality, compliance, and consistency, making AI models effective and safe for real-world use. By leveraging annotated data and advanced AI, radiology can achieve faster and more precise diagnoses, supporting truly personalized patient care.
Post Your Ad Here

Comments