The Role of Vibramycin Antibiotic in Clinical Practice
Emily’s progression through medical school brought her deeper into clinical rotations, each providing rich insights into medicine's practical realities. Vibramycin continued to emerge regularly, reinforcing her appreciation for the antibiotic’s versatility. This particular rotation—infectious diseases—would highlight precisely why Vibramycin had become a mainstay antibiotic among physicians worldwide.
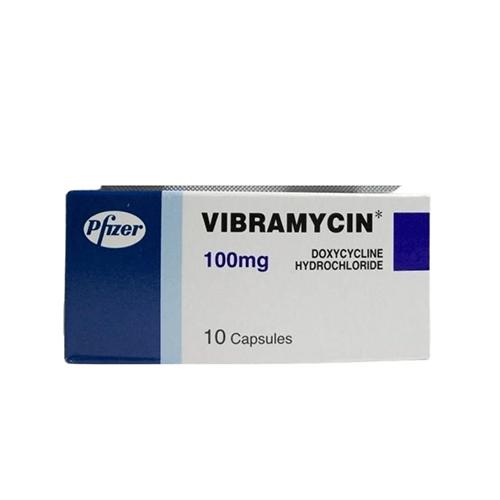
Her attending physician, Dr. Alex Conrad, a renowned infectious disease specialist, briefed the students at the start of their rotation. "You'll quickly notice," he began with a relaxed smile, "Vibramycin—known chemically as doxycycline—is one of our most trusted antibiotics. Its wide-ranging effectiveness against multiple infections makes it a staple in infectious disease management."
Emily listened intently, already familiar yet eager to see Vibramycin’s practical clinical applications unfold.
On their first day of rounds, Emily followed Dr. Conrad closely as they entered the room of Rachel Summers, a young woman diagnosed with atypical pneumonia. Rachel, looking pale and exhausted, greeted them with weary eyes.
After reviewing Rachel’s history, Dr. Conrad turned gently toward her. "We're starting you on Vibramycin, an antibiotic particularly effective against the organism causing your pneumonia. It penetrates deeply into the lung tissues, helping clear the infection efficiently."
Rachel nodded, clearly comforted by Dr. Conrad’s confident yet reassuring approach.
Afterward, Emily asked Dr. Conrad privately, "Why did you specifically select Vibramycin over other antibiotics for Rachel’s pneumonia?"
He replied warmly, "Good question, Emily. Vibramycin is uniquely effective against atypical bacteria, especially Mycoplasma pneumoniae and Chlamydophila pneumoniae, which other antibiotics might struggle to control. Its tissue penetration and intracellular effectiveness make it perfect for treating respiratory infections that linger despite standard treatments."
Emily carefully absorbed Dr. Conrad’s explanation, recognizing how each choice made in clinical practice depended on deep understanding, patient presentation, and antibiotic characteristics.
Days later, Emily encountered another patient—James Walker—a man in his forties suffering from severe, persistent acne. He’d tried numerous topical treatments without significant improvement, and dermatologists recommended an oral antibiotic approach.
Dr. Conrad carefully examined James, then explained, "Vibramycin has shown excellent results treating persistent inflammatory acne. Its anti-inflammatory properties, alongside antibacterial action, significantly reduce acne severity."
James seemed hopeful yet hesitant. "Is it safe to use antibiotics for skin conditions long-term?"
Dr. Conrad smiled calmly. "Good question. With Vibramycin, we often use it short-term initially—three to four months—during the flare-up. The goal is not long-term antibiotic use, but effective inflammation control, allowing skin to heal. Once your condition improves, we’ll reevaluate."
Emily appreciated Dr. Conrad’s balanced explanation. It highlighted the responsible use of antibiotics, emphasizing effectiveness without ignoring safety.
Later that day, Emily reflected deeply. Vibramycin’s widespread application fascinated her. Its role went far beyond merely treating infections—it included preventive medicine as well. Curious, she asked Dr. Conrad about Vibramycin’s use in malaria prophylaxis, another important indication she'd read about in recent literature.
Dr. Conrad responded enthusiastically. "Exactly, Emily. Because Vibramycin disrupts protein synthesis in Plasmodium parasites—the organism causing malaria—it is frequently prescribed as a preventive medication for travelers visiting malaria-endemic regions. It's affordable, effective, and generally well-tolerated by travelers."
Emily envisioned the importance of this application, especially for patients traveling internationally or those working in remote areas.
Over the weeks, Emily saw Vibramycin used for various infections: Lyme disease, chronic bronchitis, urinary tract infections, and even sexually transmitted diseases like chlamydia. In each case, she observed how clearly physicians and patients trusted its consistent effectiveness.
But one afternoon, Emily witnessed an important scenario highlighting antibiotic stewardship's importance. A patient, Mrs. Harris, came to the clinic requesting antibiotics for what seemed to be a mild viral infection.
Dr. Conrad patiently explained, "While Vibramycin is an excellent antibiotic, it's effective only against bacterial infections—not viral ones. Unnecessary antibiotic use could contribute to antibiotic resistance, a growing global health concern."
Mrs. Harris appeared confused. Emily gently stepped in, simplifying further, "Antibiotics like Vibramycin won't help against viral infections like the common cold or flu. Taking them unnecessarily makes bacteria resistant, potentially making future infections harder to treat."
Mrs. Harris nodded appreciatively. "Thank you, that makes sense now."
Afterwards, Dr. Conrad quietly praised Emily’s sensitive, clear communication. "That was perfectly handled. Antibiotic stewardship—knowing precisely when to prescribe or withhold medications—is a critical part of responsible medicine."
Inspired, Emily proposed an initiative within the clinic to educate patients about responsible antibiotic use, with Vibramycin as an example due to its popularity. Her project received enthusiastic support from faculty and peers.
During subsequent weeks, Emily conducted brief, patient-friendly workshops explaining antibiotic resistance clearly and practically. She explained how Vibramycin, though highly effective, needed careful prescribing practices to maintain its future usefulness. Patients welcomed these explanations, often thanking Emily for making complicated medical concepts understandable and relatable.
Toward the end of the rotation, Dr. Conrad approached Emily, expressing genuine appreciation. "Your initiative has significantly impacted patient understanding. Clarifying why responsible antibiotic use matters—and specifically using Vibramycin as an example—has noticeably improved compliance and patient satisfaction."
Emily felt deeply gratified. Her journey exploring Vibramycin antibiotic had again highlighted the profound human element in medical practice. She realized that antibiotics weren’t merely powerful medications—they represented a delicate balance between clinical efficacy, patient communication, responsibility, and trust.
As her rotation concluded, Dr. Conrad warmly summarized Emily’s contributions. "Your deep exploration into Vibramycin exemplifies the true heart of medicine—balancing science, empathy, and education. The lessons you've learned here will guide you toward becoming a physician your patients trust deeply."
Emily left the rotation inspired, carrying profound insights about Vibramycin’s role—not just medically, but as a catalyst to educate, inform, and empower patients in their own care. Her knowledge was no longer merely academic; it was personal, practical, and compassionate.
She knew clearly now that true medical excellence involved more than knowing when and how to prescribe. It required understanding patients’ experiences, recognizing antibiotics like Vibramycin’s vast capabilities and limitations, and above all, deeply valuing the human relationships she would continually nurture as a future physician.
Post Your Ad Here
Comments